QUESTIONS? GIVE US A CALL! 1-866-778-5890
FREE SHIPPING - On all orders -
QUESTIONS? GIVE US A CALL! 1-866-778-5890
FREE SHIPPING - On all orders -
PULSE OXIMETER INFORMATION
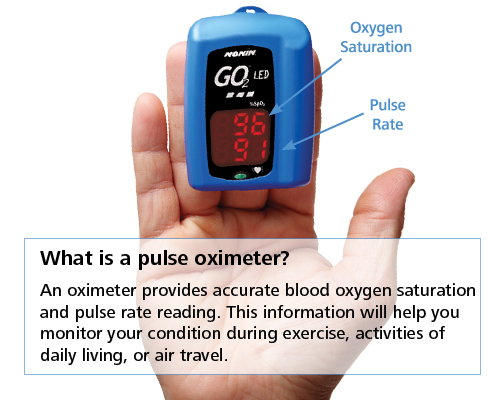
What is apulse oximeter?
Pulse oximeters are medical devices used to measure the oxygen level (or oxygen saturation SpO2 %) and heart rate in the blood. Pulse oximeters are considered to be a noninvasive, painless, general indicator of oxygen delivery to the tissues. Oximeters can acquire SpO2 and heart rate readings from thefinger, earlobe, forehead, toe, wrist or nose.
Oxygen in the air is breathed into the lungs. The oxygen then passes into the blood where the majority of the oxygen attaches to hemoglobin (a protein located inside the red blood cell) for transport in the bloodstream. The oxygenated blood circulates to the tissues.
Pulse oximeter technology utilizes the light absorptive characteristics of hemoglobin and the pulsating nature of blood flow in the arteries to aid in determining the oxygenation status in the body. First, there is a color difference between arterial hemoglobin saturated with oxygen, which is bright red, and venous hemoglobin without oxygen, which is darker.
Second, with each pulse or heartbeat there is a slight increase in the volume of blood flowing through the arteries. Because of the increase of blood volume, albeit small, there is an associated increase in oxygen-rich hemoglobin. This represents the maximum amount of oxygen-rich hemoglobin pulsating through the blood vessels.
A clip-like device called a probe is placed on a body part, such as afinger or ear lobe, to measure the blood that is still carrying or is saturated with oxygen. The probe houses a light source, a light detector, and a microprocessor, which compares and calculates the differences in the oxygen-rich versus oxygen-poor hemoglobin. One side of the probe has a light source with two different types of light, infrared and red, which are transmitted through the finger to the light detector side of the probe.SPO Medical pulse oximeters use reflectance technology to measure oxygen saturation. The oxygen-rich hemoglobin absorbs more of the infrared light and the hemoglobin without oxygen absorbs more of the red light. The microprocessor calculates the differences and converts the information to a digital readout. This information helps the physician assess the amount of oxygen being carried in the blood and evaluate the need for supplemental oxygen.
The respiratory system is made up of the organs involved in the interchanges of gases, and consists of the:
nose
pharynx
larynx
trachea
bronchi
lungs
The upper respiratory tract includes the:
nose
nasal cavity
ethmoidal air cells
frontal sinuses
maxillary sinus
larynx
trachea
The lower respiratory tract includes the lungs, bronchi, and alveoli.
What are the functions of the lungs?
The lungs take in oxygen, which cells need to live and carry out their normal functions. The lungs also get rid of carbon dioxide, a waste product of the body's cells.
The lungs are a pair of cone-shaped organs made up of spongy, pinkish-gray tissue. They take up most of the space in the chest, or the thorax (the part of the body between the base of the neck and diaphragm).
The lungs are enveloped in a membrane called the pleura.
The lungs are separated from each other by the mediastinum, an area that contains the following:
the heart and its large vessels
trachea (windpipe)
esophagus
thymus
lymph nodes
The right lung has three sections, called lobes. The left lung has two lobes. When you breathe, the air enters the body through the nose or the mouth. It then travels down the throat through the larynx (voice box) and trachea (windpipe) and goes into the lungs through tubes called main-stem bronchi.
One main-stem bronchus leads to the right lung and one to the left lung. In the lungs, the main-stem bronchi divide into smaller bronchi and then into even smaller tubes called bronchioles. Bronchioles end in tiny air sacs called alveoli.
Reasons to use Pulse Oximeters
Pulse oximeters may be used to assess the adequacy of oxygen levels (or oxygen saturation) in the blood in a variety of circumstances such as surgery, other procedures involving sedation (e.g., bronchoscopy), adjustment of supplemental oxygen as needed, effectiveness of lung medications, and patient tolerance to increased activity levels. Other reasons may include, but are not limited to, the following:
mechanical ventilation - use of a ventilator to support breathing
sleep apnea - periods of cessation of breathing during sleep
medical conditions, such as heart attack, congestive heart failure, anemia, lung cancer, asthma, or pneumonia
Risks of using a Pulse Oximeter
Pulse oximetry is a quick, noninvasive method of measuring oxygen saturation in the blood. Risks associated with using a pulse oximeter are minimal and rare.
Prolonged application of the probe may cause tissue breakdown at the application site. Skin irritation may result from the adhesive used in adhesive-containing probes.
Use of pulse oximeters in cases of smoke or carbon monoxide inhalation is contraindicated, because oximetry cannot distinguish between normal oxygen saturation in the hemoglobin and the carboxyhemoglobin saturation of hemoglobin that occurs with inhalation of smoke or carbon dioxide.
There may be other risks depending upon your specific medical condition. Be sure to discuss any concerns with your physician prior to the procedure.
Certain factors or conditions may interfere with the results of the test. These include, but are not limited to, the following:
decreased blood flow to the peripheral vessels
light shining directly on the oximetry probe
movement of the area to which the probe is attached
severe anemia (decreased red blood cells)
extreme warmth or coolness of the area to which the probe is attached
recent injection of contrast dye
smoking tobacco
Function
A blood-oxygen monitor displays the percentage of arterialhemoglobin in theoxyhemoglobin configuration. Acceptable normal ranges are from 95 to 100 percent, although values down to 90% are common. For a patient breathing room air, at not farabove sea level, an estimate of arterial pO2 can be made from the blood-oxygen monitor SpO2 reading.
A pulse oximeter is a particularly convenientnoninvasive measurement instrument. Typically it has a pair of smalllight-emitting diodes (LEDs) facing aphotodiode through a translucent part of the patient's body, usually a fingertip or an earlobe. One LED is red, withwavelength of 660 nm, and the other isinfrared, 905, 910, or 940 nm. Absorption at these wavelengths differs significantly between oxyhemoglobin and its deoxygenated form; therefore, the oxy/deoxyhemoglobin ratio can be calculated from the ratio of the absorption of the red and infrared light. The absorbance of oxyhemoglobin and deoxyhemoglobin is the same (isosbestic point) for the wavelengths of 590 and 805 nm; earlier oximeters used these wavelengths for correction for hemoglobin concentration.[2]
The monitored signal bounces in time with theheart beat because the arterialblood vessels expand and contract with each heartbeat. By examining only the varying part of theabsorption spectrum (essentially, subtracting minimum absorption from peak absorption), a monitor can ignore other tissues or nail polish, (though black nail polish tends to distort readings)[3] and discern only the absorption caused by arterial blood. Thus, detecting a pulse is essential to the operation of a pulse oximeter and it will not function if there is none.
[edit]
Advantages
A pulse oximeter is useful in any setting where a patient'soxygenation is unstable, includingintensive care, operating, recovery, emergency and hospital ward settings,pilots in unpressurized aircraft, for assessment of any patient's oxygenation, and determining the effectiveness of or need for supplementaloxygen. Assessing a patient's need for oxygen is the most essential element to life; no human life thrives in the absence of oxygen (cellular or gross). Although a pulse oximeter is used to monitor oxygenation, it cannot determine the metabolism of oxygen, or the amount of oxygen being used by a patient. For this purpose, it is necessary to also measurecarbon dioxide (CO2) levels. It is possible that it can also be used to detect abnormalities in ventilation.
However, the use of a pulse oximeter to detecthypoventilation is impaired with the use of supplemental oxygen, as it is only when patients breathe room air that abnormalities in respiratory function can be detected reliably with its use. Therefore, the routine administration of supplemental oxygen may be unwarranted if the patient is able to maintain adequate oxygenation in room air, since it can result in hypoventilation going undetected.
Because of their simplicity and speed, pulse oximeters are of critical importance inemergency medicine and are also very useful for patients with respiratory or cardiac problems, especiallyCOPD, or for diagnosis of somesleep disorders such asapnea andhypopnea. Portable battery-operated pulse oximeters are useful for pilots operating in a non-pressurized aircraft above 10,000 feet (12,500 feet in the US)[4] where supplemental oxygen is required. Prior to the oximeter's invention, many complicatedblood tests needed to be performed. Portable pulse oximeters are also useful for mountain climbers and athletes whose oxygen levels may decrease at highaltitudes or with exercise. Some portable pulse oximeters employ software that charts a patient's blood oxygen and pulse, serving as a reminder to check blood oxygen levels.
[edit]
Limitations and Advancements
Oximetry is not a complete measure of respiratory sufficiency. A patient suffering from hypoventilation (poorgas exchange in thelungs) given 100% oxygen can have excellent blood oxygen levels while still suffering fromrespiratory acidosis due to excessive carbon dioxide.
It is also not a complete measure of circulatory sufficiency. If there is insufficientbloodflow or insufficient hemoglobin in the blood (anemia), tissues can sufferhypoxia despite highoxygen saturation in the blood that does arrive.
A higher level ofmethemoglobin will tend to cause a pulse oximeter to read closer to 85% regardless of the true level of oxygen saturation. It also should be noted that the inability of two-wavelength saturation level measurement devices to distinguishcarboxyhemoglobin due tocarbon monoxide poisoning from oxyhemoglobin must be taken into account when diagnosing a patient in emergency rescue, e.g., from a fire in an apartment. A PulseCO-oximeter measures absorption at additional wavelengths to distinguish CO from O2 and determines the blood oxygen saturation more reliably.
[edit] Increasing usage
According to a report by Frost & Sullivan entitled U.S. Pulse Oximetry Monitoring Equipment Market, US sales of oximeters were worth $201 million in 2006. The report estimated that oximeter sales in the US would increase to $310 million annually by 2013.[5]
In 2008, more than half of the major internationally-exporting medical equipment manufacturers inChina were producers of pulse oximeters.[6]
In June, 2009,video game companyNintendo announced an upcomingperipheral for theWii console, dubbed the "Vitality Sensor," which consists of a pulse oximeter. This marks the onset of the use of this device for non-medical, entertainment purposes.[